Following the recent conclusion of the Oncology Care Model (OCM) on June 30, 2022, the Center for Medicare and Medicaid Innovation (CMMI) began the application process for its Enhancing Oncology Model (EOM) to further transform oncology care. Furthering its push toward value-based healthcare, CMMI developed a framework that holds physician group practices (PGP) accountable for the total cost of care (TCOC) during six-month episodes without disrupting participants’ revenue cycle. As with other CMMI programs, understanding the framework is critical, and this article seeks to clarify the complexities of beneficiary attribution. Below is a standard timeline detailing the structure of an episode under EOM.
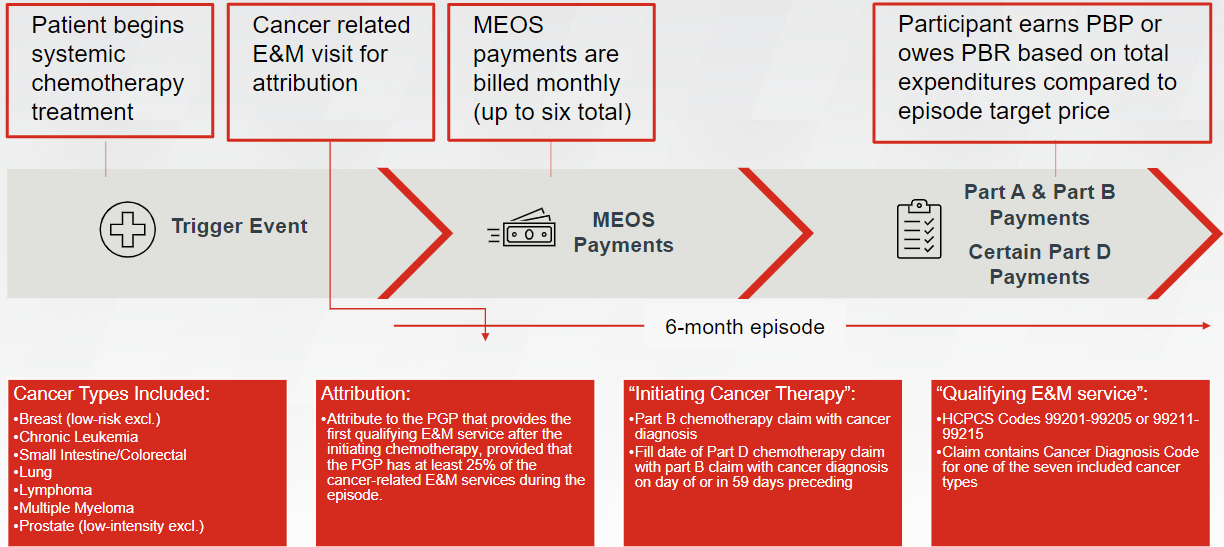
Episodes will begin with a trigger event occurring the day a patient begins receiving systemic chemotherapy for one of seven included cancer types: breast, chronic leukemia, small intestine/colorectal, lung, lymphoma, multiple myeloma, and prostate. At a more detailed level, an episode may begin with either of two different types of trigger events:
- Part B chemotherapy claim with a cancer diagnosis; or
- Part D chemotherapy claim with a corresponding Part B claim with a diagnosis code for cancer on the day of, or in the 59 days preceding, the fill date on the Part D drug claim
Episodes span six months following the trigger event and are attributed to the PGP (through one of the PGP’s providers) that provides the first qualifying evaluation and management (E&M) visit, provided that the attributed PGP has at least 25% of the cancer-related E&M services during the episode.
Participants may bill a Monthly Enhanced Oncology Services (MEOS) payment per included Medicare beneficiary for the provision of enhanced services required as part of the model’s participant redesign activities. Billing Medicare for MEOS is optional and can be billed either in real-time or within 12 months following date of service. MEOS payments total $70 per beneficiary per month (PBPM) for up to six months. Participants may bill an additional $30 PBPM for providing services to beneficiaries dually eligible for both Medicare and Medicaid. Over the course of an episode, participants may receive a maximum of $420 in MEOS payments per beneficiary or $600 per dually eligible beneficiary. For the purposes of TCOC calculation, each $70 MEOS payment will be included in total expenditures; however, the additional $30 for dually eligible beneficiaries will not be included in total expenditures.
Participants’ performance is determined by comparing their aggregated TCOC to a target benchmark amount. Based on savings and chosen risk arrangement, participants either earn a performance-based payment (PBP), owe a performance-based recoupment (PBR), or fall into the so-called neutral zone in which no reconciliation payments are made. EOM offers participants the choice between two risk arrangements—one with minimal risk and another with nominal risk. In either risk arrangement, PBP or PBR is calculated semi-annually for all episodes within a particular Performance Period.
Understanding the framework of EOM episodes will be critical to successful execution of the oncology program. Participants have an opportunity to earn significantly more reimbursement for qualifying oncology services. FORVIS can help healthcare organizations navigate and implement EOM by providing industry experience and data tools to help proactively monitor performance.
If you have any questions or need assistance, please reach out to a professional at FORVIS or submit the Contact Us form below.

