Introduction
In the last few years, BPCI-A policies have changed significantly, leading to varying degrees of participation and performance. However, our FORVIS team has seen great success stories from this Alternative Payment Model (APM) for clients who have embraced BPCI-A as an opportunity to gain experience in value-based care as it has led to new revenue streams, partnerships, and improved patient outcomes.1
Background of BPCI-Advanced
At its inception, BPCI-A brought new opportunities for hospitals and physician group practices to share financial gains with the Centers for Medicare and Medicaid (CMS) for successfully coordinating care and reducing CMS expenses incurred during a 90-day episode. As a voluntary model, BPCI-A allows qualified providers to apply and select specific episode groups in which to participate. In the application process, participants select from more than 30 predefined inpatient and outpatient clinical episodes, i.e., sepsis, spinal fusion, cardiac arrhythmia, etc. Each BPCI-A patient has a unique target price established based on the type of clinical episode, patient characteristics, and coded comorbidities prior to hospitalization. Participants that spend less than the target price in aggregate earn a financial reward; participants that spend more pay a financial penalty while all financial incentives are subject to quality results. This approach yields favorable results for many BPCI-A participants, as many participants select episodes for which they had a historically positive performance and advantageous target price fundamentals.
To learn more about the history of BPCI-A, read our article: The Evolution of BPCI-Advanced.
The significant policy changes made over the last five years led to varying levels of financial success in the model for participants. However, many participants have been successful through their disciplined execution of data-driven decision making and incremental improvements to care coordination and spend reduction.
Case Study: Self Regional Healthcare
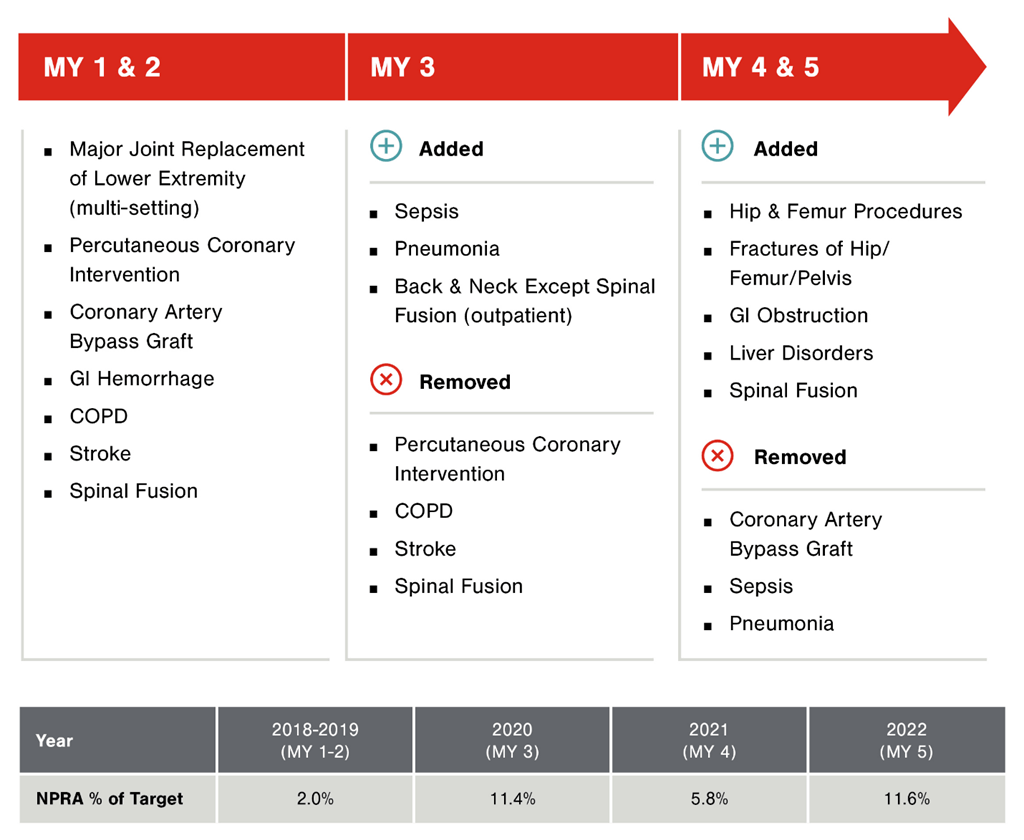
A 358-bed acute care hospital in South Carolina, Self Regional (“Self”), engaged FORVIS to support its initial application to BPCI-A in 2018 and has been actively participating in the model for five years. Beginning with enrollment in mostly procedure-based episode groups, Self earned a positive Net Payment Reconciliation Amount (“NPRA”) for the initial assessment period of October 2018 through December 2019. Leading into both 2020 and 2021, Self again engaged FORVIS to analyze the historical baseline data to determine if additional episode groups projected favorable performance. Through this analysis of historical performance as well as internal assessments of their care coordination capabilities, provider alignment, and relationships with post-acute providers, Self’s BPCI-A participation has evolved significantly, yielding increasingly profitable performance and improved care coordination.
Since beginning its participation in the Model, Self has earned more money than it’s spent on BPCI-A, and has achieved net positive performance in all model years to date. Self’s success in BPCI-A is largely due to the team’s dedication to executing on the following key strategies:
- Engaging a BPCI-A Steering Committee that meets monthly to review the claims data prepared by FORVIS and to discuss areas of opportunity and strategies for improvement, identifying issues down to the patient level.
- Using data to identify improvement opportunities, like post-acute utilization and readmissions. In 2018-2019, Self identified instances in which patients were utilizing inpatient rehab facilities (“IRF”) more often than other similar hospitals for the same diagnoses. Through a series of root-cause analyses and a focus on improving discharge planning and care coordination, Self has reduced its IRF utilization for BPCI-A patients by more than 50%, while also continuing to provide excellent patient care. As Self reduced IRF utilization, the 30-day readmission rate for BPCI-A patients did not change, and Self was even able to improve its CMS Patient Safety Indicator (PSI 90) scores.
- Implementing interdisciplinary rounding on patient floors to discuss each patient’s care plan with physicians, nursing, and other staff, including discharge instructions, discharge destination, and other patient needs.
- Deploying a BPCI-A care navigator to follow each patient post-discharge, calling patients to ensure they’re attending follow-up appointments with their primary care provider, reviewing medications, and performing root-cause analyses on all readmissions.
- Evaluating new episodes for enrollment each time CMS released historical baseline data in 2018, 2019, and 2020. Partnering with FORVIS, Self re-selected episode groups based on both historical performance and its confidence in its ability to reduce expenditures on these patients in the future.
“The data we’ve obtained through participating in BPCI-Advanced has helped us make informed care interventions and generated the necessary buy-in from our physicians, administrators, and department-level staff,” said Dr. Phillip Baker, Chief Medical Revenue Officer of Self.
Self continues to look for opportunities to improve upon its performance as it regularly reviews the BPCI-A claims data. As an example, Self recently identified opportunities to improve capture of hierarchical condition categories (HCCs) on BPCI-A patients enrolled in surgical bundles. With the help of FORVIS’ Monthly Manager analytics tool, Self was able to pull a complete listing of BPCI-A patients with missing HCCs to begin conversations and education with their surgeons.
“Going forward, our goal is to be the best at providing high-quality care for patients while also creating value for payors,” said Baker. “Participating in BPCI-A has prepared us to go down this path, moving us into more value-based arrangements as we seek to lead our market in this arena.”
As Self prepares to re-select its episode groups for 2024, its leaders are energized to find more opportunities to expand its value-based care efforts in other service lines, knowing that the healthcare environment is tying more reimbursement to quality and outcomes measures.
“We know that value-based arrangements are becoming more important in the reimbursement environment, and if we can’t adapt to the changing market, we won’t survive,” said Courtney Baker, BPCI-A Care Navigator.
Final Thoughts
As many healthcare organizations prepare to enroll or re-enroll in BPCI-A in 2024, it will be critical for each to consider its current care coordination capabilities and identify any gaps that may hinder success in the model.
For more than ten years, FORVIS has served as a trusted advisor to various bundled payment programs and value-based care organizations. In the course of FORVIS’ work, its professionals provide essential services to hundreds of bundled payment candidates to navigate participation, strategies for success, and financial opportunities. Like Self Regional, FORVIS has many clients that have achieved significant financial gains and continue to look for new bundled payment opportunities. FORVIS’ team of professionals has deep subject-matter specialization in the strategies that are proven to drive success in the model, and these same specialists are prepared to help interested applicants through program decision support, strategy development, best practice implementation, and provider alignment.
For questions or to learn more, please reach out to a FORVIS professional or submit the Contact Us form below.
- 1The statements contained in this article are solely those of the authors and do not necessarily reflect the views or policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this article.

